Speaker 1 (00:00):
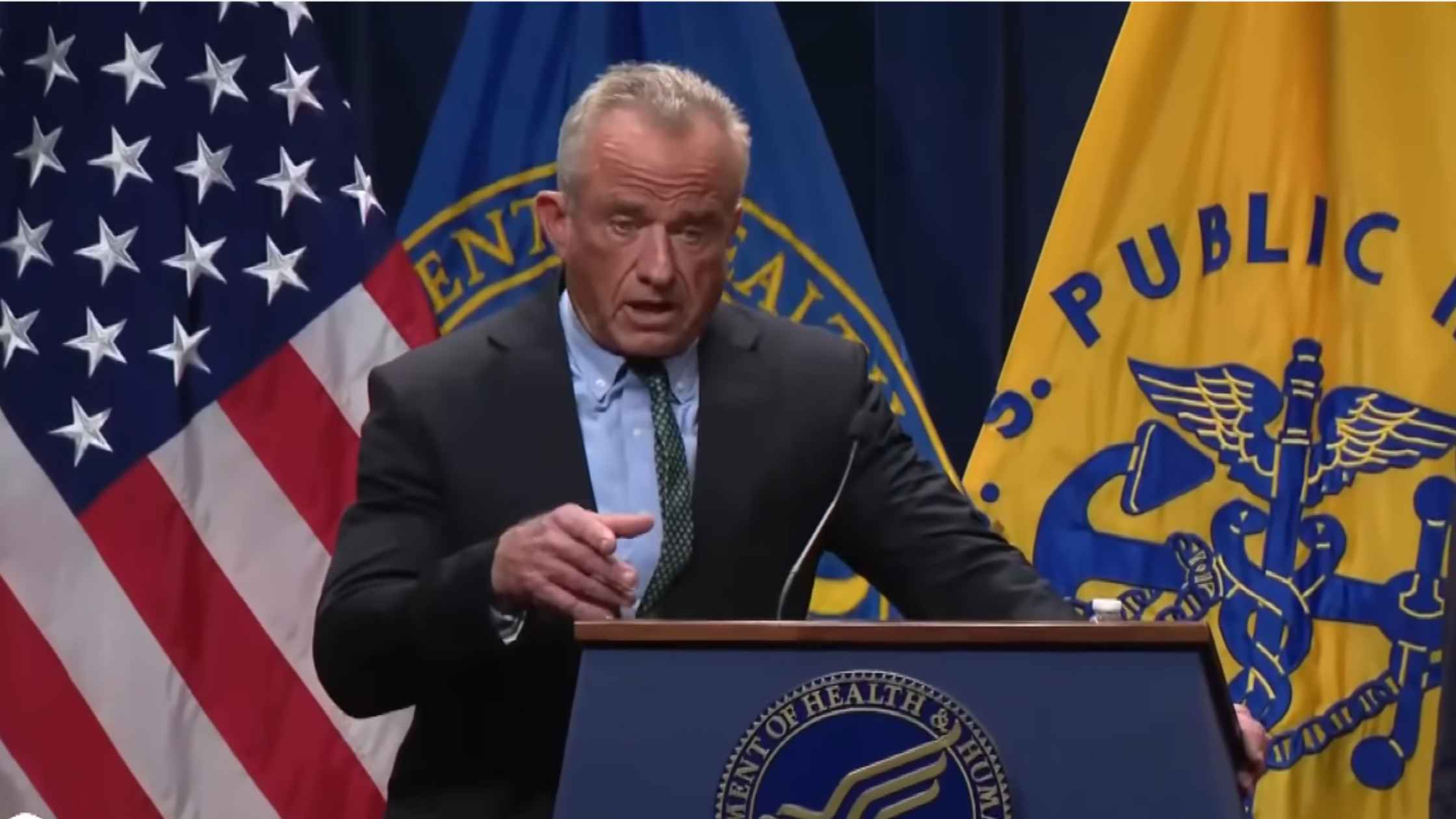
I now welcome HHS Secretary, Robert F. Kennedy Jr.
Robert F. Kennedy Jr. (00:17):
Good afternoon everybody. Across our country, millions of Americans struggle to afford essential medicines. Families are rationing prescriptions, seniors are skipping doses, and parents are facing heartbreaking choices between paying for medication or putting food on their tables. This is not acceptable of the United States of America. For decades, Americans accepted a fair deal in pharmaceuticals. A company earns a temporary monopoly for an innovative drug, and once the patent expires, cheaper generics enter the market. That system established by the 1984 Hatch-Waxman Act, works for traditional chemistry-based drugs. Proving a generic is the equivalent, is straightforward. If it's the same act of ingredient, the same effect, same safety, it gets approved. But that bargain broke down with biologic drugs, medicines made from living cells.
(01:20)
When Congress wrote the Biologics Price Competition and Innovation Act, the pharmaceutical industry rigged the rules. Between 2007 and 2009, big Pharma spent hundreds of millions of dollars lobbying to make biosimilar approval far more difficult and expensive. They claimed that biologics were too delicate, that they were too mystical to allow true generics. They compared them during these lobbying sessions to find wines. Each batch supposedly depended upon its unique grapes, the tannin content of its soils, the terrain, the humidity, the genius and personal touches of wizardry, to achieve the unique aromatic and flavor complexity of its terroir. It was all clever marketing. None of it was based on science.
(02:18)
Then to block pharmacists and doctors from switching patients to lower cost options, the lobby invented a fake distinction between biosimilars and interchangeable biosimilars. The result has been sky-high costs, endless red tape, and a biosimilar market that still lags far behind Europe's. It can cause hundreds of millions to us, federal taxpayers, just to bring one biosimilar to American patients. That changes today.
(02:52)
Under President Trump's leadership, we are ending this unscientific and corrupt system. We're cutting through the barriers that protect monopolies and opening the gates to affordable life-saving medicine for the American people. One of the biggest drivers of these crushing costs is the price of prescription drugs, of course, and especially biologic drugs. These are complex medicines made, as I said, from living cells that treat cancer, autoimmune diseases, and rare disorders, that affect millions of Americans. Biologics make up only 5% of our prescription, but they account for more than half of our drug spending. Between 2013 and 2021, our spending on biologics more than doubled, from 100 billion to 260 billion. By 2024, it reached 407 billion.
(03:48)
Some biologics cost patients up to $500,000 a year or even more. That's not a healthcare system, it's a hostage crisis. Why are these drugs so expensive? Because for too long, government bureaucracy and regulatory barriers have protected monopolies and stifled competition. The FDA's outdated and burdensome approval process, has slowed down the entry of biosimilars, the lower cost, equally safe alternatives to brand-name biologics. And even when biosimilars do get approved, current laws often prevent pharmacists or patients, from substituting them for the patients who would benefit from a more affordable option. That all ends today.
(04:38)
Today the FDA is taking bold, decisive action to break down these barriers and open the markets for real competition. The agency will release new draft guidance for companies developing biosimilars, guidance that reflects modern science and common sense. Under this new framework, companies may not always need to conduct large expensive human trials, when advanced testing can already prove that biosimilars work just as effectively and just as safely as the original drug. The FDA will also consolidate several outdated guidance documents into one streamlined rule book, for cutting unnecessary red tape, reducing uncertainty, and making it easier for innovators to bring the safe, affordable biosimilars to the market. These changes will also help ensure that more biosimilars are considered interchangeable, allowing pharmacists to substitute them just like they do with traditional generic drugs. The result will be more competition, lower prices, and faster access to life-saving medicines. And we know this approach works.
(05:54)
Since 2015, biosimilars have already saved Americans over $56 billion, 20 billion in 2024 alone. On average, biosimilars cost 50% less than their brand-name counterparts, and their entry into the market drives down brand-name prices by another 25%. That's real relief for patients, families, and for the American taxpayer, but America still lags far behind Europe and other nations. In Europe, for example, regulators have approved more than twice as many biosimilars as the United States, and patients there are paying far less for many of these treatments. These reforms reflect President Trump's directive, to restore competition, to empower patients, and lower drug cause for every American. This victory for patients or innovation and for common sense.
(06:55)
We're replacing bureaucracy with science. We're replacing monopolies with competition. And we're replacing despair with hope. Every American, regardless of income or zip code, deserves access to affordable, effective, and safe medicine. The actions we're taking today move us closer to that goal, and advance our mission to make America healthy again. Thank you all very much. And now I'd like to welcome the genius behind this innovation, FDA Commissioner Dr. Marty Makary. There you are, Marty.
Marty Makary (07:34):
Thank you. Great. Thank you Mr. Secretary, and thank you for your commitment to lowering drug prices for everyday Americans. We're interested in everyday Americans. There's been a lot of talk about healthcare costs, a lot of talk about reducing drug prices. But as you've seen from the Oval Office, thanks to the good work of Dr. Mehmet Oz, and his team at CMS, you're now seeing medications come down to a price point of pennies on the dollar. Reforms that have been discussed for 35 years, but have never translated into action and most favored nation status pricing. I'm happy to contribute, with our reform at the FDA, to this incredible movement to lower drug prices, not by one or 2%, but significantly. If you haven't noticed, healthcare costs have gone way up since the promise of the Affordable Care Act to make the price of health insurance premiums more affordable, lowering them by $2,500. Within seven years, they went up by $2,500. The opposite direction of the promise.
(08:38)
The fastest growing area of health care spending in the United States is drug spending. And the fastest area of drug spending increases is with this new class of medicines called, biologics. That's because they are derived from cell lines. It's an expensive process to develop biologics, so they are naturally going to cost more, but not a thousand times more, not 10,000 times more. I've seen biologics work wonders as Dr. Oz has in the hospital. Our patients, I've seen cancer patients get biologics with results almost visible during the treatment. It's worked wonders. Amazing benefits for patients with autoimmune diseases. Patients after transplant surgery. Patients with all sorts of cancers, rare and common. Biologics are amazing. And the biologic drug makers are not bad guys, they're good guys.
(09:42)
We are doing a lot to promote innovation with biologics, streamlining and modernizing the FDA. Our new pilot to get decisions out in weeks. Reducing animal testing requirements, which reduces R&D time and the time to come to market. But today, we are talking
Marty Makary (10:00):
… specifically about the price tag on biologics, up to $200,000, almost a quarter million dollars for some. Who's got that kind of money? Now, some people might say, "Look, I'm not paying for it. My employer's paying for it." Or, "I'm not paying for it. Medicare pays for it." Well, guess where that money comes from? It comes from the everyday American worker. That comes from their paycheck. The money for these expensive biologics comes from their paycheck deduction for health insurance. If your employer's paying for part of your health insurance, guess where that money comes from? It comes from a pool of money allocated to wages and benefits. It comes from you, the American worker.
(10:44)
When you get a paycheck, there's a deduction for a Medicare Excise Tax. All of that money is getting towards these expensive biologics. And look, we should be paying top dollar for top products. But this administration is interested in the 80% of Americans that live paycheck-to-paycheck. This administration has not forgotten, as we have in the academic ivory towers, at the panels on conferences, in the hollowed chambers of healthcare experts discussing healthcare reform, we have not forgotten that 50% of Americans have less than $500 of cash on hand. And when you have less than $500 of cash on hand and your car breaks down, or you get a bill or you have a co-pay for a biologic, that can be catastrophic.
(11:35)
Well, there are low cost alternatives to these expensive biologics. The good news is there are low cost alternatives. Unfortunately, there are far fewer on the market than should be because of regulatory red tape hurdles. There's about 76 that the FDA has approved since we started approving biosimilars. Think of biosimilars as the generic version of the expensive biologics. We have 76 that we've approved in 10 years. Probably should have been 200 or 300. But there's a series of onerous requirements that the FDA has had, making the process long and expensive for the makers of these biosimilar equivalents.
(12:20)
Today, the FDA is issuing draft guidance to eliminate the onerous requirement of comparative studies that have historically been associated with biosimilars and their approval. We don't have these additional requirements for generics. Moving forward, we're not going to have them for biosimilars. This reform will take the five to eight year timeframe to bring a biosimilar to market and cut it in half. It will also save companies about $100 million in their development costs. That'll take the cost down from 200 million down to 100 million or 250 million down to 150 million. I'm giving you real numbers that companies have shared with me on their costs. Lower prices for drug development means lower R&D costs and lower drug prices for everyday Americans.
(13:12)
Today, the FDA is also announcing its plans to issue final guidance on interchangeability, something the Secretary just described, eliminating the bureaucratic switching studies that have been required. When a doctor prescribes a branded small molecule, the patient and their pharmacist can have that substituted out for a generic small molecule. But not so with biosimilars. We are taking a strong stand to advance and promote interchangeability. Congress has been talking about this for a long time, but we're taking action. We encourage them to act, but in the meantime, we're not wasting time. When Humira, the powerful biologic, which works wonders, came off patent, it took seven years for a biosimilar to come to market. Why? Because of these burdensome, onerous, bureaucratic red tape requirements in part at the FDA.
(14:09)
The fundamental problem in healthcare is that we have non-competitive markets. It's something we don't talk about. It's a sacred cow topic. But the solution is to convert them to competitive markets. We want to see more biosimilars. We want to see more competition, more choices. When the first biosimilar came on the market seven years after Humira's patent expired, prices really didn't go down. Call it an implied collusion of prices, but it takes typically until two or three biosimilars come to market to see the prices really drop. That's why we need to reduce the hurdles and get more biosimilars on the market.
(14:49)
Right now, we're not doing well. We walked into a mess. Of all the biologics, the expensive biologics that, again, are amazing, that are about to come off patent in the next 10 years, only 10% have a biosimilar in development. It should be 30% or 40% or more. These reforms have tremendous implications for everyone and every stakeholder in healthcare. I want to thank the staff at the FDA. They've been wanting to do this for a long time. People have been talking about it and we're doing it. The implications are broad. This series of reforms has implications for community pharmacies, PBMs, hospitals, and Medicare and Medicaid. And so because of the enormous implications for Medicare and Medicaid and the billions of dollars in potential savings, I'm now going to introduce the smartest doctor I have ever met, Dr. Mehmet Oz. Mehmet, why don't you come up? Thanks.
Dr. Mehmet Oz (15:54):
God bless you. Thanks.
Marty Makary (15:55):
Thanks. Thanks.
Dr. Mehmet Oz (15:57):
We are stuck with the bill. It's going up 9% this year for Medicare, increasing faster than that in Medicaid, and it's increasing about 9% for the commercial insurance. And to address these increasing costs, you have to have brave leadership. Secretary Kennedy, god bless you for always messaging that at every level and it rubs off on us in today's case in point. Marty, you're very kind to call me all the things you've said, but I can say without question, running the FDA requires a brave human being. You've got to be able to withstand tremendous pressures, and I want to congratulate the FDA Commissioner Marty Makary because he's been able to push for change that has been waiting for decades to occur. Secretary Kennedy went through these numbers. Just put that 1984 date in your mind. That's when Congress acted and said, "These things called generics exist." It took a long time to make them 91% of the medications that we currently use, saving billions of dollars to the American taxpayer.
(16:51)
But there's a group called the catchy named, Association of Accessible Medicines. How many of you have heard of that name? I didn't think so. One person put their hand up too. One and a half people. Exactly. Compelling. It's a group of state scientists, doctors, technology people, pharmacists. They gave Marty three standing ovations today for announcing what you just heard. That doesn't happen in academic circles. I don't think I've ever gotten a standing ovation three times, certainly in one presentation. It speaks to the stunning impact that this will have on the industry. Of course, I want to thank the President for messaging that he supports rapid change and encouraging us to go out there and make a difference.
(17:30)
And this whole-of-government approach that Secretary Kennedy has been pushing for, which Marty, myself, Jay Bhattacharya, who runs the NIH, many others in this wonderful agency have been unified around has allowed us to achieve things in our short stay here that are unimaginable. As Secretary Kennedy said in the Oval Office a week and a half ago, "No one thought most favorite nation drug pricing would be possible." It turns out not only is it possible, it's probable under the leadership of Chris Klump, John Brooks, and others. There's been remarkable advances in getting pharmaceutical companies, who are not bad guys, guys who are involved in innovation and want to make sure we make the lifesaving choices out there available, can strive and make that happen, but at an affordable price.
(18:12)
And we've asked these companies to stand up, be counted, be patriotic, and give us pricing that allows the American public to not have to choose between groceries and lifesaving medications. And pharmaceutical companies have come to the table to help fix a wrong, but they got two problems. All of us, in fairness, have two problems. The first is access. A study just this year, just this year it came out from a prestigious group, one in seven Medicare beneficiaries skip their medications. You should never have to choose between medications in this country of abundance. And when you're choosing in a country that believes non-scarcity, but in bountiful ability to do what you want in life, it causes some very expensive complications, which we all still pay for, readmissions to hospitals and, of course, it can lead to deaths as well if we don't take medications which we believe could save your life.
(19:02)
Now, at the same time, we have an access issue. We don't want to compromise innovation, and the President and the Secretary have been allowed on this and Marty has defended the need for innovation in the industry. The FDA has gone through a lot of painstaking work to ensure that they protect against hindering the cutting edge of industry to allow lifesaving medications to come to market. But if you've got 20 years on a patent and let's say 12 years after your biologic is approved, you should be allowed to recoup that money in that period of time. But once that patent's over, insurgents should be allowed to enter the marketplace to appropriately compete. That's what the ecosystem of fairness should represent.
(19:41)
That's what's been hindered with this 40 year history of one by one having to break through barriers, with this being one of the largest and perhaps the final major barrier to ensure that what started with the Hatch-Waxman Act can now reach full fruition and allow the intent of Congress to be heard widely, which is generic products
Dr. Mehmet Oz (20:00):
The biosimilars when they're appropriately to be released, because patents have expired, should allow a competition not a crony capitalism to run the market. The current system has slowed the ability of insurgents to enter the market, and that stops today under the leadership of Dr. Makary. Now, CMS's job is to pay the bills. We've focused on improving reimbursement models, we've done all kinds of innovative things under Abe Sutton's leadership at CMMI. We're working with the private sector. A good example of that is just on Monday, one of the leading pharmacy benefits management companies, the middleman company of this country, announced after discussions with us that they will voluntarily change their business model. If you didn't see this news, it is big. As the Secretary Kennedy tweeted out on it, this is allowing this industry to transform itself from a rebate-based system where you hide the ball to one of ultimate transparency where everyone's going to see, including employers, who will no longer be able to hide behind PBMs as they sometimes allow extra funds to be channeled back to them through the rebate system.
(21:01)
Now everyone's going to know what the numbers are, and to make sure that's true, TrumpRx is going to publish the numbers of all the medications and their pricing, including the generics and biosimilar competitors so individuals can make the right choice for them and will have options. The power to convene of this agency has been shown in other areas as well. I won't go through the entire list, but it has been remarkably effective, but it doesn't work unless we have the brave actions of the FDA, the Commissioner's leadership, to go out there and put real drugs in the hands of real doctors taking care of real patients. The increased transparency is going to make a huge difference but I have three asks, and I ask this on behalf of CMS, but I think it applies to the entire agency.
(21:43)
First, I'm asking patients right now to push for the medications you think make sense for you, using the interchangeability options that the Commissioner is offering today. You have the ability to ask, "Why can't I get a cheaper biosimilar medication if it's just as good as the biologic that I've been paying a lot of money for or my insurance company's been paying for?" Second big ask, I'm asking plans, insurance plans to consider thoughtful design changes to allow low-cost biosimilars to be more accessible to their patients. There have been historically reasons, including the rebate model, why that hasn't been allowed, or endorsed, or supported. We don't want money paid on the side to determine whether a plan is made available to the employees of a company, we are not going to allow Medicare anymore. And the third big ask is to governors. If you can hear my voice now, please listen carefully. Medicaid money spent on these biosimilars will dramatically reduce the cost that states have to shoulder for Medicaid. That allows Medicaid to exist healthily with access to all the medications that can be life-saving and life-changing. At the same time, not crowd out education and other social services. Take advantage of the work done in Washington to allow your state capital to push for the bountiful access to Medicaid-funded drugs at the right price. God bless you all. The boss.
Speaker 2 (23:09):
All right, we'll take questions from the press. Please keep your questions to what we're here talking about today, and also if you can give your outlet, first name, and last name. Go ahead.
Speaker 3 (23:24):
Zach, Brennan with Endpoints News.
Speaker 2 (23:25):
And there's a microphone.
Speaker 3 (23:26):
Oh, thank you. Zach Brennan with Endpoints News. So you offered the example of Humira where we now see 10 biosimilar competitors, some priced at more than 80% off, and yet AbbVie still controls the vast majority of the market. What are you going to do for specific cases like that where we see an influx of biosimilars and yet they're still not gaining traction on the market? And then on interchangeability, I know the FDA has already approved biosimilars and as interchangeable without running the switching studies, what is new that's coming out today?
Marty Makary (24:00):
Yeah, first of all, there have been waivers of those switching studies that have been granted by the FDA. Now we're going to issue clear final guidance that those are not required. The uncertainty makes it difficult for drug developers. As you know, Zach, with capital markets, they want predictability. And so knowing that now they can invest in a biosimilar's development and have a timeframe of coming to market, from being at the drawing board to actually coming to market, of now two and a half to five years instead of five to eight years, and we think we can also shave off some of the time that it takes for the FDA to approve biosimilars, we've identified ways that we can streamline that process as we are with other drugs. So you're correct in that some of those waivers have been issued, so we are going to make it very clear now in our procure guidance.
(24:56)
With Humira, the Humira example that you described, let's be honest about what's going on sometimes. The branded biologic manufacturer is paying the PBM to make sure that biosimilars are not added to that formulary. We're calling for increased transparency. You can see we talk every day, we talk all the time, this is a top priority for Dr. Oz to increase transparency and to make biosimilars a priority. And so he's asking many of the stakeholder groups that he has access to take a look at biosimilars. That includes Medicare Advantage plans, it includes Medicaid plans, it includes Medicare Part B and D, biosimilars are in both parts.
(25:45)
So I think we're not going to sugarcoat things, we're going to be very honest about what we see in the marketplace, and I think you're identifying something that we need to call out. Now. You can come up with protectionist strategies that try to regulate bad behavior, we can do that, we can talk about the merits of that, or we can create more intense competition and let the market forces do some of that. So when Humira had its biosimilar come out, seven years later, it should be about two years, or if the biosimilar starts in development earlier like it does in Europe, maybe one year or half a year, but when you have that gap, it allows a longer period of no competition. So we want to see more competition and we want to see more innovation both.
Speaker 4 (26:40):
Hi, Emily Kopp with the Daily Caller. This is for Dr. Makary. You said that FDA wanted to do this before now. Why didn't it happen? What forces were at play there? And to follow up on Zach's question, my recollection of the TrumpRx executive order is that it proposed FTC action perhaps if they didn't come to the table. Some of the protectionist strategies you're talking about, could that see FTC action also?
Speaker 5 (27:08):
Go ahead.
Marty Makary (27:12):
Okay, thanks. Well, first of all, at the FDA, there are great ideas that just have not gotten daylight. Take for example, our work on removing the nine petroleum-based food dyes from the US food supply. They've been talking about that for 35 years, they had a citizens petition, and two business days before this new administration, they took action on one of them. Well, within weeks we took action on all nine. So there are great ideas that just have not gotten daylight at the FDA, and this is one of them. People have seen the mired bureaucracy that has stalled biosimilars, and so we spend a lot of time listening to people on the front lines, asking them what big ideas do you have and what we can do that's meaningful that has an impact? And so we've announced a ton of these reforms, reducing animal testing requirements, been talking about that for 20 years. Now we've got good computational modeling and we have our roadmap public, and we're going to make another announcement on animal testing requirement elimination probably next week.
(28:18)
On the TrumpRx, TrumpRx is genius because you can bypass healthcare's middlemen. If you like Health Care's middlemen marking up the price of drugs and taking kickbacks from the manufacturers, use the current system, but if you want another option to shop for a price to see if that price is better, that's what TrumpRx is for,` it allows direct purchasing.
Speaker 6 (28:41):
Thanks, David Lim of Politico. You mentioned that this final guidance is coming soon, can you put a timeline on that? And then secondly, I wanted to ask about the role of Congress. Interchangeability obviously is in statute, could you talk about whether you think that this move requires them to take any action to prevent litigation risk from biopharmaceutical companies?
Marty Makary (29:10):
First on the final guidance, I would say three to six months. On the interchangeability, it's very complicated because we have the opportunity at the FDA to designate a biosimilar as interchangeable. We're saying basically we think all biosimilars should be interchangeable, and then states have their own rules on whether or not patients need to be consented or not for substitution. So we're planting a flag saying, we want interchangeability, we promote it, we encourage it, and look, I would love it if Congress solidified this in law, but we're not going to wait for them. Thank you.
Speaker 2 (29:49):
Go ahead.
Speaker 7 (00:00):
Speaker 7 (30:00):
Hi, Paige Cunningham, Washington Post. This question is for Secretary Kennedy. The president has called for breaking up the MMR vaccine into three separate shots. I'm wondering, are you going to be-
Robert F. Kennedy Jr. (30:10):
Can you speak up a little, please?
Speaker 7 (30:11):
Yeah, the president has asked to break up the MMR vaccine into three separate shots. Is that something you're going to direct ACIP to consider or take action on?
Robert F. Kennedy Jr. (30:22):
We're looking at the feasibility of that now.
Speaker 7 (30:26):
Can you say anything more on that?
Speaker 8 (30:32):
Hi, Daniel Payne with STAT. You're saying here that-
Speaker 11 (30:35):
Can you speak up?
Speaker 8 (30:36):
Daniel Payne with STAT. You're saying here that you want to reduce the evidence that's required to get biosimilars in the market, but the administration has argued again and again that there isn't enough evidence for vaccines which are biosimilars. Can you help me understand why more evidence is needed for some things and other things you want less evidence?
Robert F. Kennedy Jr. (30:55):
So, can you just repeat that? You said that… Can you speak up a little?
Speaker 8 (31:01):
Of course. In this announcement, you're saying that biosimilars, you want to reduce the evidence needed for them to come to market, but previously, the administration has said that vaccines and other biosimilars, there's not enough evidence for them to be on the market in the first place. You suggest that you need more evidence. Can you help explain the differential there?
Robert F. Kennedy Jr. (31:25):
Well, with the long-chain molecules like biosimilars, the brand drug has been thoroughly tested. It's been safety tested. It's been efficacy tested. It's been proven. And we're going to implement the same procedure that is used for small-molecule drugs, which is if the active ingredient works, if it's been proven safe, if it's been proven efficacious, then you ought to be able to get it on the market right away, the same as small molecule.
(31:58)
With vaccines, the issue is very different because none of the vaccines currently recommended for children, with one exception, the COVID vaccine, has ever been tested in pre-licensing trials for safety in a randomized placebo-controlled trial. So, the starting point is very, very different with vaccines than it is for biologics.
Speaker 9 (32:32):
Thank you very much. Arthur Jones II with ABC News. Can you just talk about, Secretary Kennedy, the amount or the significance this announcement will have on struggling American families, as you've mentioned at the top of this? And secondly, I've spoken to a number of Republican senators, actually, about the linkage between pregnant mothers using Tylenol and this risk of autism or other health disorders in unborn children. And one prominent senator told me that the evidence there is weak and there's no relationship. Can you respond to that?
Robert F. Kennedy Jr. (33:06):
For Tylenol?
Speaker 9 (33:07):
For Tylenol.
Robert F. Kennedy Jr. (33:08):
Okay, on your first question, I mean there's a good example that we worked on recently. We recently put together an agreement in South Carolina and now some other states, the private insurers and for Medicaid and Medicare to pay for sickle cell anemia treatment. The cost of that treatment is a million dollars. It cures sickle cell anemia, but it's a million dollars. If we could get a generic drug, a biosimilar, that does the exact same thing for a fraction of the cost, we can make that treatment available in every state.
(33:51)
Right now, it is barely economic for the insurance companies because they think that maybe the long-term treatment of somebody with sickle cell anemia is going to cost more than that million dollars and it's right on the borderline. So, if we could cut that in half, it would be a no-brainer for every single state to adopt it.
(34:18)
With Tylenol, we've all said from the beginning that the causative association with between Tylenol given in pregnancy and the perinatal periods is not sufficient to say it definitely causes autism, but it is very suggestive. And it's suggestive in animal studies and core blood studies and observational studies from nation to nation. And so, there should be a cautious approach to it and that's why our message to patients, to mothers, to people who are pregnant, to the mothers of young children is, "Consult your physician." And we have asked physicians to minimize the use to when it's absolutely necessary.
Speaker 10 (35:15):
Hi, Jacob Gardenswartz with Scripps News. Thanks for doing this. You mentioned at the top that you want medications to be affordable, effective and safe for Americans. We're speaking today on the day that window shopping began in the Affordable Care Act program on those marketplaces and that shows that unless those tax credits are extended, those subsidies, the average plan will increase for Americans by somewhere around 115%. Do you believe that Congress should extend those subsidies, so that most Americans do not receive significant increases in their premiums?
Dr. Mehmet Oz (35:45):
Where'd you get that 115% number from?
Speaker 10 (35:47):
Kaiser Family Foundation.
Dr. Mehmet Oz (35:49):
They retracted that. That data was run inappropriately. They changed the messaging on it. Go back and look at the website. Here's the truth, the window shopping is already revealing that the average American who's on the ACA between 100% and 400% of poverty level is going to pay $50 total next year. It's going to be $13 more than this year. So, there can be a lot of hair pulling and scratching, mudslinging. But the fundamental reality for most Americans is that although it is an increase in spend, that's not the big issue. The big issue is the fundamental flaws within the ACA as they were created 15 years ago. We want government reopened, so that we have people working, running the numbers, trying to help experts, actuarials, insurance company experts, to try to figure out more holistic ways of dealing with the bigger challenges that we face in America with increasing costs, which I don't think the enhanced premium tax subs, which were created for COVID, designed for COVID, there were short-term, initially for a just a year then extended until this year just to get through COVID. And I think we all agree that COVID has passed, so therefore, COVID-era subsidies should also pass.
Speaker 10 (37:06):
Can I just follow up on that? So, this is from the CMS release that went out this morning, announcing window shopping. You noted that in 2026, nearly 60% of eligible re-enrollees will have a plan, but in their chosen category at or below 50% after those tax credits, that's down from 83% in 2025. So, that's a pretty significant number of Americans who will not be at that $50 a month range. Are you concerned about those Americans being able to afford their premium payments?
Dr. Mehmet Oz (37:30):
I'm always concerned about Americans being able to afford payments. The question then becomes what's the best way to fix the problem? The ACA promised many things that just were not delivered on. And I don't know why $50 is the magic number. I picked that, by the way, because that's historically the number that's been thrown out there. Half the people on the ACA, half the people on the ACA today, listen carefully, filed no claims last year. None. Zero. So, I have to ask myself, you should be as well, if I had insurance, why would I never use it? The concern that has been raised is that a large number of the 12 million people who never use their insurance last year may not legitimately have the insurance, know they have the insurance, want to have the insurance, so we have many bigger problems. And to fix the issues, we have to have Congress and this agency, CMS, but the entire HHS staff back at work. You can't do that if we're furloughed because of, I think, partisan bickering in Congress.
Speaker 11 (38:29):
Great. Thank you, everybody.